What is The Added Value of Hemoptysis in our Decision Rules for PE?
September 23, 2022
Written by Bo Stubblefield
Spoon Feed
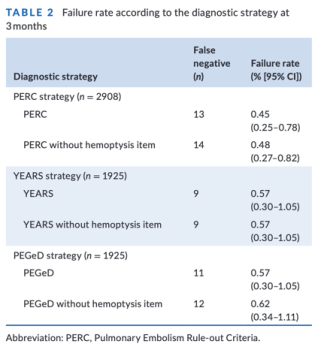
Removing the “hemoptysis” item from PERC1-4, YEARS,5-7 and PEGeD8 clinical decision tools (CDTs) did not significantly increase diagnostic failure in a cohort of patients at low risk for acute pulmonary embolism (PE).
Why does this matter?
Over-imaging for suspected PE in US emergency departments (ED) is a public health problem. Diagnostic yield for PE has been reported at ~1-3% in newer studies (3% in this analysis).9,10 This ED prevalence of acute PE is lower than what has been reported in previous validation studies.11,12 The three aforementioned CDTs, as well as two scores of clinical probability (Wells & Geneva) all include the “hemoptysis” item in their respective checklists. Hemoptysis is neither sensitive nor specific to PE, with its principal etiologies including respiratory infections, neoplasia, and bronchial dilation.13 Is hemoptysis still a relevant clinical item to adapt the diagnostic workup for PE given the lower prevalence of PE in the ED? Can we remove the hemoptysis item from these CDRs – increase the testing threshold of low-risk patients, potentially relieving some patients of additional testing?
*Cough cough* what is that? Blood? Yeah…don’t count that.
This was a post-hoc analysis of two prospective cohort studies (PROPER and PERCEPIC) evaluating CDTs in a population of low-risk patients with suspected acute PE.3,4 A total of 2,968 patients were included in the analysis. Patients were followed up at 3 months and very few were lost to follow up. Table 2 below gives the deets. The performance of the YEARS and PEGeD rules were not altered by the removal of hemoptysis. The performance of the PERC score was not significantly reduced.a As secondary outcomes, risk stratification by Wells’ and Geneva remained similar without the hemoptysis item. The removal of hemoptysis from all CDT did not result in a clinically significant reduction in diagnostic CT imaging.
aAuthor’s note: This study does not provide enough argument to remove the hemoptysis item from PERC. There were three PE cases (8.1%) in the 37 patients with hemoptysis in this cohort. The prevalence of PE in patients with hemoptysis and no other PERC criteria was 6.6%. Most of these patients with suspected PE don’t check the hemoptysis box, but the authors suggest that including hemoptysis item in the different CDRs is of limited value for patients presenting primarily with hemoptysis. Frankly, I agree. These patients should not follow usual diagnostic strategies, and application of the different CDR may not reduce the number of CTs in this subset of patients.
Another Spoonful
- Check out our recent JF on the diagnostic strategy of PERC+YEARS+Age-adjusted D-dimer. It’s magical!7
- Quick reference of PE CDTs:
Source
Evaluation of the “hemoptysis” item in clinical decision rules for the diagnosis of pulmonary embolism in the emergency department. Acad Emerg Med. 2022 Jul 30. doi: 10.1111/acem.14574.
Works Cited
- Kline JA, Mitchell AM, Kabrhel C, Richman PB, Courtney DM. Clinical criteria to prevent unnecessary diagnostic testing in emergency department patients with suspected pulmonary embolism. Journal of thrombosis and haemostasis : JTH 2004;2:1247-55.
- Kline JA, Courtney DM, Kabrhel C, et al. Prospective multicenter evaluation of the pulmonary embolism rule-out criteria. Journal of thrombosis and haemostasis : JTH 2008;6:772-80.
- Freund Y, Cachanado M, Aubry A, et al. Effect of the Pulmonary Embolism Rule-Out Criteria on Subsequent Thromboembolic Events Among Low-Risk Emergency Department Patients: The PROPER Randomized Clinical Trial. Jama 2018;319:559-66.
- Penaloza A, Soulie C, Moumneh T, et al. Pulmonary embolism rule-out criteria (PERC) rule in European patients with low implicit clinical probability (PERCEPIC): a multicentre, prospective, observational study. Lancet Haematol 2017;4:e615-e21.
- van der Hulle T, Cheung WY, Kooij S, et al. Simplified diagnostic management of suspected pulmonary embolism (the YEARS study): a prospective, multicentre, cohort study. Lancet 2017;390:289-97.
- Kabrhel C, Van Hylckama Vlieg A, Muzikanski A, et al. Multicenter Evaluation of the YEARS Criteria in Emergency Department Patients Evaluated for Pulmonary Embolism. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine 2018;25:987-94.
- Freund Y, Chauvin A, Jimenez S, et al. Effect of a Diagnostic Strategy Using an Elevated and Age-Adjusted D-Dimer Threshold on Thromboembolic Events in Emergency Department Patients With Suspected Pulmonary Embolism: A Randomized Clinical Trial. Jama 2021;326:2141-9.
- Parpia S, Takach Lapner S, Schutgens R, Elf J, Geersing GJ, Kearon C. Clinical pre-test probability adjusted versus age-adjusted D-dimer interpretation strategy for DVT diagnosis: A diagnostic individual patient data meta-analysis. Journal of thrombosis and haemostasis : JTH 2019.
- Kline JA, Garrett JS, Sarmiento EJ, Strachan CC, Courtney DM. Over-Testing for Suspected Pulmonary Embolism in American Emergency Departments: The Continuing Epidemic. Circ Cardiovasc Qual Outcomes 2020;13:e005753.
- Dhakal P, Iftikhar MH, Wang L, et al. Overutilisation of imaging studies for diagnosis of pulmonary embolism: are we following the guidelines? Postgrad Med J 2019;95:420-4.
- Wells PS, Anderson DR, Rodger M, et al. Derivation of a simple clinical model to categorize patients probability of pulmonary embolism: increasing the models utility with the SimpliRED D-dimer. Thrombosis and haemostasis 2000;83:416-20.
- Le Gal G, Righini M, Roy PM, et al. Prediction of pulmonary embolism in the emergency department: the revised Geneva score. Ann Intern Med 2006;144:165-71.
- Abdulmalak C, Cottenet J, Beltramo G, et al. Haemoptysis in adults: a 5-year study using the French nationwide hospital administrative database. Eur Respir J 2015;46:503-11.

