Trauma in Pregnancy – New WEST Guideline and Algorithm
November 2, 2022
Written by Seth Walsh-Blackmore
Spoon Feed
The primary survey and standard initial interventions are the same. Here is how a viable pregnancy changes the algorithm beyond that.
Why does this matter?
Severe trauma is uncommon in pregnancy, so there is less experience in resuscitating these challenging patients. Data quality is lower, as there are few RCTs. This expert guidance helps with these challenging situations.
What to expect when they’re expecting.
A preplanned obstetric trauma response team and cart should be available if your center receives trauma patients. This should include both maternal and neonatal resources.
For any female trauma:
Do a pregnancy test for ages >10 and <55 years and consider even outside this range. Pregnancy status does not alter the primary survey and initial diagnostics, including chest and pelvis x-rays.
For any pregnant trauma patient:
Consult OB. Give Rhogam if Rh status is unknown or Rh negative. Consider a left lateral tilt or decubitus for hypotension, especially when > 20 weeks. Use O-negative blood. Administer oxygen and minimize pressors. Place chest tubes 1-2 rib spaces higher than normal. Screen for domestic violence. Assume viability if 23 weeks gestation by history or fundus above the umbilicus. If available, OB determines viability.
For pregnant trauma with viable fetus:
- Set-up fetal monitoring after the primary survey. Expand the secondary survey for frank vaginal bleeding/injury or fetal parts but defer a speculum exam.
- An unstable mother is the priority and gets standard resuscitation. If not responding, proceed to advanced interventional management.
- Be prepared for a C-section following any occlusive intervention such as REBOA, cross clamping, or IR embolization of the pelvis. C-section can be done during an ex-lap.
- Perimortem C-section outside the OR is indicated only with imminent maternal death and a viable fetus.
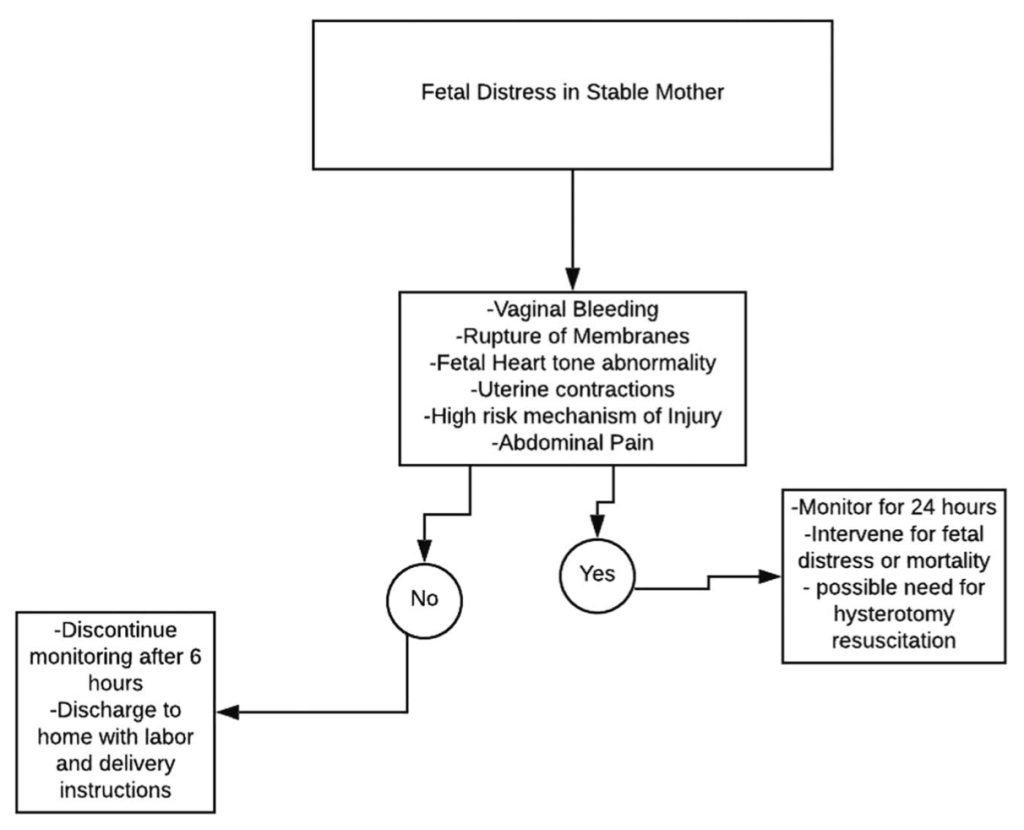
- Responsive/stable mothers with signs of fetal distress should be on fetal monitoring for at least 24 hours, with both trauma and OB available. While addressing non-life threatening injuries, be judicious with radiologic imaging and mindful of contraindicated medications.
- Stable mothers without abdominal pain, high-risk mechanism, or signs of fetal distress need monitoring for at least 6 hours followed by a fetal ultrasound.
Here are the algorithms.

Source
Pregnancy in trauma-A Western Trauma Association algorithm. J Trauma Acute Care Surg. 2022 Oct 1;93(4):e139-e142. doi: 10.1097/TA.0000000000003740. Epub 2022 Jul 8.


One thought on “Trauma in Pregnancy – New WEST Guideline and Algorithm”